Heart failure with preserved ejection fraction is unique to each individual, requiring a personalized treatment plan and closely monitored care. Show
 Multiple factors can lead to heart failure with preserved ejection fraction (HFpEF), a condition in which the heart muscle pumps blood normally but still doesn’t meet the body’s nutrition and oxygen requirements. MORE FROM MICHIGAN: Sign up for our weekly newsletter Ingeborg Ludeking knows this all too well. Atrial fibrillation, pulmonary hypertension, an enlarged heart and sleep apnea were among the conditions on a long list of health concerns for the 78-year-old. Her case isn’t unusual. Most patients with HFpEF — pronounced “hef-pef” — also have several other illnesses, says Scott Hummel, M.D., M.S., who directs the University of Michigan Frankel Cardiovascular Center’s HFpEF program along with Matthew Konerman, M.D. “HFpEF develops when one or more chronic medical conditions gradually change the structure and function of the heart and blood vessels,” says Hummel. “These changes stiffen the heart and make it more difficult for the heart to fill appropriately, thus limiting the amount of blood pumped with each beat.” Despite Ludeking’s many health challenges, the resident of Clinton Township, Michigan, was able to enjoy a relatively active life until four years ago, when she began finding it difficult to breathe. “I couldn’t take more than 10 steps before having to stop to catch my breath,” she recalls. Warning signsHFpEF symptoms often include:
Risk factorsUnderlying conditions or factors associated with HFpEF include:
A heart catheterization in 2015 confirmed Ludeking’s HFpEF diagnosis. Her HFpEF risk factors were high, says Hummel, noting that the condition is becoming more widespread as the country’s population ages and the associated risk factors become more common.  Treatment for HFpEFHummel says treatment for most patients with HFpEF includes controlling blood pressure and reducing excess fluid in the body that can cause swelling or shortness of breath. SEE ALSO: How to Avoid a Heart Attack While Shoveling Snow That isn’t always enough, however. And reactive measures are often unique to the individual. “HFpEF is a very complex illness, and there isn’t one treatment that works for all patients,” Hummel says. “When a patient is diagnosed, we have to sort through the individual aspects of the underlying conditions that contribute to it. We often also use information from diagnostic tests such as echocardiography, heart catheterization, stress testing and cardiac MRI to design the best treatment plan for each patient’s particular situation. “We promote lifestyle modification, including exercise and dietary interventions, which can improve quality of life in HFpEF patients. Each of our patients has a nurse case manager assigned to monitor and support them, and direct pager access to the physician directing his or her care,” says Hummel. A place in her heartLudeking was treated with diuretics to reduce the fluid affecting her heart and lungs, beta-blockers to keep her heart rate stable and blood thinners to prevent stroke. Her treatment protocol has proved successful. “Dr. Hummel and his team have made a big difference in my well-being. I feel better today than I’ve felt in a long time,” says Ludeking, who keeps active by riding a stationary bike, tending to her yard and cleaning her home. “U-M has a special place in my heart,” she says. Photos by Leisa Thompson RELATED ARTICLESCurr Cardiol Rev. 2015 Feb; 11(1): 42–52. Heart failure with preserved ejection fraction (HFpEF) is a common clinical syndrome associated with high rates of morbidi-ty and mortality. Due to the lack of evidence-based therapies and increasing prevalence of HFpEF, clinicians are often con-fronted with these patients and yet have little
guidance on how to effectively diagnose and manage them. Here we offer 10 key lessons to assist with the care of patients with HFpEF: (1) Know the difference between diastolic dysfunction, diastolic heart failure, and HFpEF; (2) diagnosing HFpEF is challenging, so be thorough and consider invasive hemodynamic testing to confirm the diagnosis; (3) a normal B-type natriuretic peptide does not exclude the diagnosis of HFpEF; (4) elevated pul-monary artery systolic pressure on echocardiography in
the presence of a normal ejection fraction should prompt considera-tion of HFpEF; (5) use dynamic testing in evaluating the possibility of HFpEF in patients with unexplained dyspnea or exer-cise tolerance; (6) all patients with HFpEF should be systematically evaluated for the presence of coronary artery disease; (7) use targeted treatment for HFpEF patients based on their phenotypic classification; (8) treat HFpEF patients now by treating their comorbidities; (9) understand the importance of
heart rate in HFpEF—lower is not always better; and (10) do not forget to consider rare diseases (“zebras”) as causes for HFpEF when evaluating and treating patients. Taken together, these 10 key lessons can help clinicians care for challenging patients with HFpEF while we eagerly await the results of ongoing HFpEF clinical trials and observational studies. Keywords: B-type natriuretic peptide, comorbidities, diagnosis, diastolic heart failure, exercise testing,
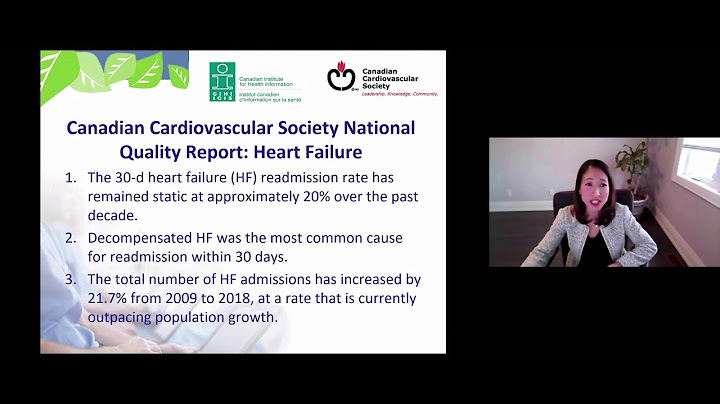
pulmonary hypertension, treatment. Heart failure (HF) with preserved ejection fraction (HFpEF) currently represents approximately 50% of HF cases and is increasingly recognized as a leading cause of morbidity and mortality
[1-3]. Recent data suggest that the prevalence of HFpEF relative to HF with reduced ejection fraction (HFrEF) is increasing at a rate of 1% per year. With the aging population and high prevalence of HFpEF risk factors such as hypertension, obesity, and diabetes
mellitus (DM), HFpEF will soon be the most prevalent HF phenotype [2]. Similarly, hospitalizations due to HFpEF have been rising relative to HFrEF [4]. Population-based studies and registries have reported that HFpEF patients are predominantly
female and elderly, with high rate of comorbidities, such as obesity, hypertension, chronic kidney disease, coronary artery disease (CAD), anemia, hyperlipidemia, DM, and atrial fibrillation [1,
5-7]. Patients with HFpEF are as functionally limited as their counterparts with HFrEF, they require frequent hospitalizations, and have generally poor quality of life
[3, 4, 8]. Survival of patients with HFpEF is poor and similar to HFrEF, with observational studies reporting a dismal 5-year survival of only
35-40% post-hospitalization for HF [2, 5], a survival rate similar to advanced, stage 3B non-small cell lung cancer [9]. In a wider variety of HF
patients (inpatients and outpatients, observational studies and clinical trials), a patient-level meta-analysis found that risk of death was higher in HFrEF compared to HFpEF; nevertheless, the overall risk of death was high in HF regardless of the underlying EF [10]. One of the key reasons underlying the high morbidity and mortality of HFpEF is the lack of evidence-based
treatments [2, 11]. These statistics highlight the pressing and unmet clinical need for new strategies for improving HFpEF quality of life and outcomes. While HFpEF clinical trials are ongoing, clinicians need help diagnosing and treating HFpEF
today. Here we report 10 key lessons for the care of patients with HFpEF, based on our experience from a novel, dedicated HFpEF clinical and research program at Northwestern University. Diastolic dysfunction (DD) is a pathophysiologic condition associated with impaired myocardial relaxation and/or decreased left ventricular (LV)
compliance, both of which can lead to elevated filling pressures [12]. Thus, DD is not a clinical syndrome and does not necessarily mean that HF is present. HF, on the other hand, refers to a clinical syndrome characterized by a classic constellation of signs and symptoms of pulmonary and/or systemic venous congestion caused by impaired ability of the heart to fill with and/or
to eject blood proportional to the metabolic needs of the body [1, 13]. HFpEF was initially termed diastolic HF [14] or HF due to DD
[15]. However, the term “diastolic HF” is suboptimal for several reasons. Diastolic HF suggests a single underlying mechanism, which is not present in all HFpEF patients [16]. Several alternative and complementary pathophysiologic mechanisms exist in HFpEF,
including longitudinal LV systolic dysfunction (despite a normal EF), pulmonary hypertension, abnormal ventricular-arterial coupling, abnormal exercise-induced vasodilation, extracardiac volume overload, and chronotropic incompetence [11, 17-25]. It should also be noted that echocardiographic evidence of DD is nearly universal in HFrEF (“systolic HF”); therefore, DD is not unique to diastolic HF [26]. Thus, diastolic HF is a subset of HFpEF (Fig.
1) and although its frequency is not well known, “isolated” or “pure” diastolic HF is most likely a rare phenomenon, as shown in a study of HFpEF pathophysiology by Prasad et al.
[27]. In this study, 1119 patients with a discharge diagnosis of HF and EF > 50% were identified using screening of inpatient electronic medical records; after several exclusion criteria, only 23 (2%) of the patients with “pure” diastolic HF met criteria for enrollment. Differentiation of diastolic dysfunction, diastolic heart failure, and heart failure with preserved ejection fraction. Abbreviations: DD—diastolic dysfunction; DHF—diastolic heart failure; HFpEF—heart failure with preserved ejection fraction; LV—left ventricular; LVEF—left ventricular ejection fraction. Using the HFpEF term reminds us to think broadly about the underlying etiologies and pathophysiologies of HFpEF in each individual patient. We use the term “huff-puff” to help patients and healthcare providers understand that HFpEF is a better, more inclusive term compared to diastolic HF, and that “huffing and puffing” (dyspnea and exercise intolerance) are the most common symptoms in patients with HFpEF. LESSON #2: DIAGNOSING HFpEF IS CHALLENGING, SO BE THOROUGH AND CONSIDER INVASIVE HEMODYNAMIC TESTING TO CONFIRM THE DIAGNOSISThe diagnosis of HFpEF can be challenging, because symptoms are nonspecific and can be explained by several alternative non-cardiac conditions, such as chronic lung disease, anemia, and chronic kidney disease [28]. Furthermore, many patients are morbidly obese and clinicians often have difficulty estimating jugular venous pressure. Echocardiographic estimation of right atrial pressure by inspection of the size and collapsibility of the inferior vena cava can also be challenging in the obese patient. As discussed below, even natriuretic peptides can be unreliable for the diagnosis of HFpEF. Finally, there is no simple index, such as a low EF, to help rule in the diagnosis of HFpEF. Thus, diagnosing HFpEF requires diligence and hypervigilance. If all else fails and there is still diagnostic uncertainty, we advocate the use of invasive hemodynamic testing to firmly establish the diagnosis of HFpEF. If cardiac filling pressures are normal at the time of invasive hemodynamic testing, one must make certain that the cardiac index is normal. If the cardiac index is low, a diagnostic maneuver such as leg raise, fluid challenge, and/or exercise should be performed to determine whether the “normal” cardiac filling pressures are truly normal. Four sets of guidelines have been published for the diagnosis of HFpEF. All of these guidelines require the simultaneous and obligatory presence of signs and/or symptoms of HF, evidence of normal LVEF, and evidence of DD [11, 14, 29-31]. As mentioned above, emphasis on DD in these guidelines does not necessarily imply the fact that DD is the only underlying mechanism of HFpEF [26]. Ultimately, presence of DD on echocardiography (especially moderate [grade 2] or worse DD, along with left atrial enlargement) simply helps with objectively documenting the presence of increased LV filling pressures. Studies have shown no statistically significant difference in the prevalence of signs and symptoms between patients with HFpEF and HFrEF. Patients with either condition often present with dyspnea on exertion, impaired exercise tolerance, paroxysmal nocturnal dyspnea or orthopnea. Each may have similar signs of HF, such as jugular venous distension, rales, S3, S4, hepatomegaly, and edema, and the 2 types of HF share similar chest radiographic findings [32, 33]. Echocardiography is considered as the single most useful diagnostic test in the evaluation of the patients with HF due to its availability and ability to provide information about cardiac anatomy, valvular structures, wall thickness, and filling pressures [34, 35]. Although there is no clear consensus, we consider a “preserved” EF to be > 50%, and also require an LV end-diastolic volume index < 97 ml/m2 as suggested previously [14, 29-31]. It is critical to remember that in a patient with signs and symptoms of HF, EF > 50%, and evidence of elevated LV filling pressure (elevated E/e’ ratio, increased left atrial volume, elevated BNP or NT-proBNP, or elevated invasive LV filling pressure) is all that is required for diagnosis of the HFpEF syndrome. Because diastolic function grading can be somewhat variable and subjective, the absence of “diastolic dysfunction” on echocardiography does not rule out the diagnosis of HFpEF as long as there is alternative objective evidence of elevated LV filling pressure at rest or with exertion. Figure (2) summarizes a diagnostic and management approach to HFpEF, with specific emphasis on CAD (see also Lesson #6 below).  Systematic diagnosis and treatment algorithm for heart failure and preserved ejection fraction (HFpEF), with specific criteria for diagnosis of coronary artery disease in HFpEF. Modified with permission from Shah SJ, Current Treatment Options in Cardiovascular Medicine, 2010; 12: 58-75. ACE—angiotensinconverting enzyme; ACS—acute coronary syndrome; ARB—angiotensin receptor blocker; BP—blood pressure; CABG—coronary artery bypass grafting; CAD—coronary artery disease; CI—chronotropic incompetence; CKD—chronic kidney disease; HF—heart failure; LV— left ventricular; LVEF—left ventricular ejection fraction; MI—myocardial infarction; PCI—percutaneous coronary intervention. LESSON #3: A NORMAL B-TYPE NATRIURETIC PEPTIDE DOES NOT EXCLUDE THE DIAGNOSIS OF HFpEFNatriuretic peptides (B-type natriuretic peptide [BNP] and NT-proBNP) provide valuable information for the diagnosis of HF [36], and elevated levels of BNP and NT-proBNP are potent predictors of adverse outcomes in HF regardless of underlying EF. The European Society of Cardiology guideline on the diagnosis of HFpEF therefore recommends the exclusion of HFpEF in the setting of normal BNP level (<100 pg/ml) [29]. However, most studies on natriuretic peptides have included patients with HFrEF, and BNP is less sensitive for the diagnosis of HFpEF, with levels that are usually lower in patients with HFpEF compared to those with HFrEF [37]. BNP levels more accurately reflect LV wall stress compared to LV filling pressures, and LV wall stress is known to be lower in HFpEF compared to HFrEF [38, 39]. Several studies have shown that patients with HFpEF can have normal BNP levels [40, 41]. We found that up to 30% of patients with HFpEF have BNP levels < 100 pg/ml despite HF signs and symptoms and invasive hemodynamic evidence of significantly elevated LV filling pressures (> 20 mmHg) [28]. Obesity, which is very common in HFpEF, is well known to be associated with low natriuretic peptide levels [42, 43], and may be one of the most important underlying reasons for the presence of normal BNP levels in some patients with HFpEF. Taken together, these findings demonstrate that while BNP levels are powerful and independent predictors of future events in patients with HFpEF, a normal BNP or NT-proBNP level cannot exclude the diagnosis of HFpEF. In patients who have signs and symptoms of HF with normal BNP or NT-proBNP, clinicians must remain vigilant and use echocardiography and/or invasive hemodynamic testing to look for alternative objective evidence of elevated cardiac filling pressures. LESSON #4: ELEVATED PULMONARY ARTERY SYSTOLIC PRESSURE ON ECHOCARDIOGRAPHY WITH A NORMAL LEFT VENTRICULAR EJECTION FRACTION? CONSIDER HFpEFLeft heart disease is the most common cause of pulmonary hypertension (PH), and patients with left heart disease-associated PH have a worse prognosis compared to patients with pulmonary artery hypertension (PAH) [44-46]. A seminal study by Lam and colleagues showed that the frequency of elevated pulmonary artery systolic pressure (PASP) among patients with HFpEF is 83% [23]. PH in patients with HFpEF is predominantly due to pulmonary venous hypertension secondary to passive congestion of the pulmonary vasculature. HFpEF comorbidities such as obesity, obstructive sleep apnea, and chronic kidney disease likely contribute to the elevated pulmonary artery pressures in HFpEF, and a small subset of HFpEF patients likely develop superimposed PAH [23, 47]. Despite its technical limitations, Doppler echocardiography has been the cornerstone of estimation of PASP given its widespread availability, portability, and ease of use. PASP estimated by echocardiography was shown to be a better predictor of HFpEF when compared to other echocardiographic parameters associated with DD such as E/e’ ratio, LA volume, and LV wall thickness [23]. Therefore, in patients with normal LVEF, elevated PASP is suggestive of HFpEF until proven otherwise, especially since HFpEF is much more prevalent than PAH. However other potential causes of PH, such as valvular heart disease, lung disease, chronic thromboembolic disease, and obstructive sleep apnea should be considered while evaluating these patients. PASP can also be elevated due to high cardiac output states (such as anemia, hyperthyroidism, cirrhosis, arteriovenous malformation) or because of increased systolic blood pressure [46]. Several clinical features can be helpful to differentiate HFpEF associated PH from PAH [48]. These features include older age, CAD, and/or systemic hypertension. Echocardiographic clues to the presence of HFpEF instead of PAH include increased E/A ratio, increased E/e’ ratio (using the lateral e’ velocity), and left atrial enlargement (especially if the left atrium is larger than the right atrium) [49]. These data suggest that in a patient with signs and symptoms of HF or possible HF (such as unexplained dyspnea), elevated PASP in the presence of a normal LVEF should prompt consideration of HFpEF, especially if other causes of elevated PASP (as detailed above) have been excluded. LESSON #5: USE DYNAMIC TESTING TO EVALUATE UNEXPLAINED DYSPNEA OR EXERCISE TOLERANCE WHEN CONSIDERING THE HFpEF DIAGNOSISPatients with early stages of HFpEF may present with exertional dyspnea and/or fatigue in the absence of signs of overt volume overload on physical examination. In addition, resting echocardiography may demonstrate only mild (grade I) DD and normal or indeterminate LV filling pressures (E/e’ ratio). Chest radiography may also be normal with lack of evidence of HF. In such patients who are at early stages of HFpEF and asymptomatic at rest, making a specific diagnosis may be challenging, and hemodynamic evaluation during exercise might be the only way to detect the hemodynamic derangements specific to HFpEF [11]. Several studies have also shown that although LVEF is “preserved” in patients with HFpEF, they can still have abnormalities in regional contractility and this leads to impaired systolic reserve due to blunted increase in contractility and LVEF during exercise [50]. Similarly, patients with HFpEF were shown to have impairment in diastolic reserve (ability to increase preload volume with no increase in filling pressures in response to exercise) [51], chronotropic reserve (ability to appropriately increase heart rate in response to exercise) [19, 20], and vascular reserve (ability to vasodilate appropriately with exercise) [50]. In a prospective study by Borlaug and colleagues, measurement of hemodynamic parameters with invasive methods during exercise was found to be helpful for accurate and specific diagnosis of HFpEF [38]. Diastolic stress testing (non-invasive echocardiographic estimates of LV filling pressures [E/e’] during rest and peak exercise) has also been shown to be useful in diagnosing exercise-induced elevations in LV filling pressure [52], and may be useful to diagnose HFpEF via exercise echocardiography. In patients with unexplained dyspnea or exercise intolerance, in whom HFpEF may be a possibility, we typically start with exercise echocardiography (including measurement of E/e’ ratio and PASP at peak stress) and cardiopulmonary exercise testing. If the cause of dyspnea is still equivocal, we proceed with exercise cardiac catheterization for further evaluation of possible HFpEF. LESSON #6: LOOK FOR CORONARY ARTERY DISEASE IN ALL PATIENTS WITH HFpEFCAD is less prevalent in patients with HFpEF compared to those with HFrEF [6]. However the frequency of CAD in HFpEF is still very high. Several epidemiologic and observational studies have documented a CAD prevalence of approximately 50% in HFpEF, although the number varies among studies [4, 6]. In addition, the presence of CAD is known to be associated with increased risk of developing HFpEF and increased mortality among HFpEF patients [53]. Both chronic CAD and acute myocardial ischemia have been associated with DD [54]. Two major mechanisms underlying the link between CAD and DD are the following: (1) impairment of active relaxation, an energy-dependent phase of diastole which is vulnerable to ischemia; and (2) alteration of the passive relaxation properties of the myocardium due to fibrosis or scarring [54, 55]. Longstanding myocardial ischemia can also induce myocardial hypertrophy and change in the extracellular matrix and this results in decreased LV compliance permanently [56]. Myocardial ischemia due to epicardial/microvascular coronary disease is also thought to be associated with decreased diastolic and/or systolic reserve in HFpEF patients [11]. Finally, by interfering with diastolic coronary filling, DD itself may also lead to myocardial ischemia [55]. CAD is a treatable condition that can play a significant role in the pathogenesis of HFpEF if present. In addition, symptoms of CAD can mimic symptoms of HF. Therefore, systematic identification of CAD is an important part of management of HFpEF [55]. Guidelines from the Heart Failure Society of America recommend evaluation for ischemic heart disease and inducible myocardial ischemia in patients with HFpEF [34]. We therefore screen for CAD in all patients with HFpEF. Given the high prevalence (pre-test probability) of CAD in HFpEF, along with the typical test characteristics of imaging-based stress testing, a negative stress test for CAD in HFpEF may not reliably exclude the diagnosis. Thus, we start with coronary angiography in all patients with HFpEF unless contraindicated (or if there is a desire to help localize ischemia prior to coronary angiography) [55]. In these cases, we perform stress testing to evaluate for the presence and extent of CAD and myocardial ischemia. Figure 2 displays our recommended diagnostic and treatment algorithm for CAD in HFpEF. LESSON #7: CATEGORIZE HFpEF PATIENTS INTO CLINICAL PHENOTYPES TO HELP DETERMINE THE BEST MANAGEMENT STRATEGY IN THE INDIVIDUAL PATIENTAll patients with HFpEF will benefit from blood pressure control, diuresis, HF education (i.e., dietary sodium restriction, fluid restriction, daily weights), management of polypharmacy and medication interactions, diagnosis and treatment of comorbidities, routine follow-up, and close interaction with primary care and other providers for management of comorbidities. For blood pressure control, we typically use a combination of carvedilol (given its vasodilating and cardioprotective properties), ACE-inhibitors/ARBs, and thiazide diuretics. For control of volume overload, we typically use bumetanide rather than furosemide given its better bioavailability. Once initial diuresis is complete, we try to minimize the loop diuretic dose to prevent over-diuresis and sympathetic activation. If volume overload is severe or resistant, we add a more potent thiazide diuretic as needed (and judiciously, to avoid electrolyte imbalances), and we have a low threshold for spironolactone, especially in patients with right heart failure. HFpEF is a heterogeneous syndrome with multiple etiologies and comorbidities. Therefore, aside from general treatment recommendations, we have found it helpful to categorize patients into clinical phenotypes to target specific therapies towards specific types of HFpEF. Table 1 lists the various clinical phenotypes of HFpEF along with specific management strategies for each subtype of HFpEF. Table 1.Management of heart failure with preserved ejection fraction (HFpEF) by phenotypic classification.
LESSON #8: IT IS POSSIBLE TO TREAT HFpEF—TREAT NOW BY TREATING UNDERLYING COMORBIDITIESOver the past decades, the prognosis of patients with HFrEF has improved significantly with the help of HFrEF-specific therapies. However, despite the use of similar pharmacological agents, prognosis of patients with HFpEF remained unchanged during the same time period [2]. Previous clinical trials with different pharmacological agents with strong evidence for benefit in HFrEF such as angiotensin converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), beta-blockers, and digoxin have all failed to show significant benefit in the treatment of HFpEF [57-62]. A recent study on the effects of spironolactone in mild HFpEF showed improvement in DD without any effect on exercise capacity, patient symptoms, or quality of life [63]. Treatment of Preserved Cardiac Function Heart Failure with an Aldosterone Antagonist (TOPCAT), a large trial of spironolactone (N=3445) in more symptomatic, advanced HFpEF is still in progress [3]. Better understanding of pathophysiology of HFpEF has identified new drug targets [64]. A small trial with a short follow-up period showed significant improvement in pulmonary pressure, right ventricular function, and LV relaxation and distensibility with the use of sildenafil in HFpEF patients who had evidence of superimposed PAH [65]. However, in the Phosphodiesterase-5 Inhibition to Improve Clinical Status and Exercise Capacity in Diastolic Heart Failure (RELAX) trial, a more recent randomized controlled trial of HFpEF (which did not require the presence of PH), sildenafil did not result in significant improvement in clinical outcomes or exercise capacity [66]. A phase 2 clinical trial of a novel agent, an angiotensin receptor neprilysin inhibitor (ARNI), showed significant improvement in NT-proBNP levels compared to valsartan in patients with HFpEF and mild-to-moderate HF symptoms [67]. Several other agents such as L-carnitine [68], I(f)-inhibition (ivadarabine) [69], and soluble guanylate cyclase activators, may also be beneficial in HFpEF. However, these novel therapeutic options require further investigation in HFpEF to determine whether they are associated with improved outcomes in Phase III trials [67]. In the absence of evidence-based therapies for HFpEF, many clinicians may feel a bit of therapeutic nihilism towards these patients. However, we can treat these patients now by treating their comorbidities. In patients with HFpEF, although morbidity and mortality are high, comorbidities drive as much of the adverse outcomes in these patients as the HF syndrome itself. In addition, in HFpEF, the number of comorbidities has been shown to be associated with increased risk for all-cause hospitalization in a dose-response relationship [70]. Therefore, clinicians should aggressively identify and treat conditions such as CAD, hypertension, diabetes, CKD and cerebrovascular disease in HFpEF because doing so may improve overall outcomes [71]. Table 2 lists several common HFpEF comorbidities and the management strategies we recommend to treat them. Table 2.Management of comorbidities in heart failure with preserved ejection fraction (HFpEF).
LESSON #9: UNDERSTAND THE IMPORTANCE OF HEART RATE IN HFpEFThere is a complex relationship between heart rate and the pathophysiology of HFpEF. Elevated resting heart rate is known to be associated with increased mortality and hospitalization in HFpEF patients [72, 73]. At the same time, chronotropic incompetence is prevalent in HFpEF and plays an important role in its pathogenesis. Traditionally, heart rate lowering agents have been suggested to be beneficial for LV filling by increasing the diastolic filling period [34]. However, in the absence of tachycardia, slowing the heart rate tends to only prolong diastasis, during which time transmitral flow is minimal or absent [11]. Studies on beta-blockers have mostly shown neutral (no benefit or harm) outcomes in HFpEF, although potential benefits exist in patients with HFpEF-CAD [74-76]. Beta-blockers may worsen exercise intolerance by exacerbating chronotropic incompetence in patients with HFpEF. Therefore, whenever possible, heart rate response to exercise should be determined with exercise testing in patients with HFpEF, and if chronotropic incompetence is present, rate adaptive pacemaker insertion may be considered to improve exercise tolerance and this may allow use of beta-blockers [55]. Some patients with advanced HFpEF (especially those with restrictive cardiomyopathies such as cardiac amyloidosis) have a fixed stroke volume (due to severe DD and severely reduced LV compliance); these patients therefore require the ability to increase heart rate in order to augment cardiac output with exercise. In this setting, permitting heart rates as high as 90-100 bpm may be beneficial, and heart rate lowering agents should be used with caution, as they may precipitate lightheadedness, dizziness, hypotension, and syncope. LESSON #10: REMEMBER THE ZEBRAS WHEN EVALUATING PATIENTS WITH HFpEFThe broad differential diagnosis of HFpEF must be considered during the evaluation of patients with known or possible HFpEF [34], especially when initial treatment strategies are unsuccessful. Careful history and detailed physical examination can help narrow the differential diagnosis. Common diagnoses such as anemia, chronic kidney disease, atrial fibrillation, CAD, valvular heart disease, pulmonary hypertension, and lung disease can all mimic HFpEF. Additionally, several “zebras” (rare diseases such as restrictive cardiomyopathies, including cardiac amyloidosis, and constrictive pericarditis) can result in the HFpEF syndrome [77]. Patients with these rare conditions often benefit from early diagnosis; therefore, clues to their presence are essential in the proper diagnosis and management of patients with HFpEF. On physical examination, Kussmaul’s sign (an increase in jugular venous pressure during inspiration) can be suggestive of restrictive cardiomyopathy, constrictive pericarditis, significant right ventricular dysfunction, or severe tricuspid regurgitation. A pericardial knock can be present in patients with constrictive pericarditis [78]. Although similarly timed within the cardiac cycle, a pericardial knock can be differentiated from an S3 by its intensity, pitch, and timing (the pericardial knock is louder, higher pitched, and slightly earlier than the S3). Periorbital purpura and bilateral carpal tunnel syndrome are clues for the diagnosis of amyloidosis [79]. The presence of low voltage QRS on electrocardiography (often times with a pseudoinfarct pattern [pathologic Q waves due to cardiomyopathy]), especially in a patient with increased LV wall thickness, should also prompt consideration of cardiac amyloidosis. Careful examination of echocardiographic findings in patients with HFpEF can provide clues to the presence of restrictive cardiomyopathy and constrictive pericarditis, as outlined in Table 3 and Fig. (3).  Doppler and tissue Doppler tracings from a 50-year-old patient with dyspnea, exercise intolerance, and preserved left ventricular ejection fraction. Panel A = Doppler imaging of mitral inflow; Panel B = tissue Doppler imaging of the septal mitral annulus. The high E velocity, high E/A ratio, short E deceleration time, and severely reduced tissue Doppler e’ and a’ velocities all point to severe (Grade 3) diastolic dysfunction. The presence of severe diastolic dysfunction with severely reduced e’ and a’ tissue Doppler velocities is highly indicative of an underlying cardiomyopathy (restrictive or infiltrative) in a relatively young patient with preserved left ventricular ejection fraction and no evidence of severe coronary disease or end-stage renal disease. This particular patient had symptoms for 2 years and had seen multiple cardiologists prior to the diagnosis of HFpEF due to biopsy-proven cardiac AL amyloidosis. She underwent chemotherapy followed by autologous stem cell transplantation and has been free of heart failure symptoms or evidence of primary AL amyloid recurrence for 5 years. Table 3.Clues for the presence of restrictive cardiomyopathy or constrictive pericarditis in patients with heart failure and preserved ejection fraction.
CONCLUSIONHFpEF (“huff puff”), a common clinical syndrome that is increasing in prevalence with the aging population, is associated with an alarmingly high morbidity and mortality. Unfortunately, the majority of multi-center randomized clinical trials have failed to identify treatments with proven benefit in quality of life or outcomes, especially in the outpatient setting. Clinicians therefore may approach HFpEF with diagnostic and therapeutic nihilism, thereby considering these patients as untreatable and difficult to manage because of the lack of guidelines and treatment options. Indeed, the Cambridge Idioms Dictionary defines “huff and puff” as follows: “to complain noisily about something but not be able to do anything about it”. It is our hope that these 10 key lessons for HFpEF will show clinicians that we can do something about HFpEF by giving them tools to help diagnose, treat, and manage these patients effectively, thereby ultimately improving outcomes. ACKNOWLEDGEMENTSAHA Scientist Development Grant (#0835488N) and National Institutes of Health (R01 HL107557). CONFLICT OF INTERESTThe authors confirm that this article content has no conflict of interest. DISCLOSURESDr. Shah reports receiving a research grant from Gilead Sciences; has served as a consultant for Bristol Squib-Myers, Bayer-Schering Pharma, and Novartis; and has received honoraria from the Pulmonary Hypertension Association. REFERENCES1. Lam CS, Donal E, Kraigher-Krainer E, Vasan RS. Epidemiology and clinical course of heart failure with preserved ejec-tion fraction. Eur J Heart Fail. 2011;13:18–28. [PMC free article] [PubMed] [Google Scholar] 2. Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355:251–9. [PubMed] [Google Scholar] 3. Shah SJ, Heitner JF, Sweitzer NK , et al. Baseline char-acteristics of Patients in the Treatment of Preserved Cardiac Function Heart Failure with an Aldosterone Antagonist (TOPCAT) Trial. Circ Heart Fail. 2013;6(2):184–92. [PMC free article] [PubMed] [Google Scholar] 4. Steinberg BA, Zhao X, Heidenreich PA , et al. Trends in patients hospitalized with heart failure and preserved left ventricu-lar ejection fraction prevalence, therapies, and outcomes. Circulation. 2012;126:65–75. [PubMed] [Google Scholar] 5. Bhatia RS, Tu JV, Lee DS , et al. Outcome of heart failure with preserved ejection fraction in a population-based study. N Engl J Med. 2006;355:260–9. [PubMed] [Google Scholar] 6. Yancy CW, Lopatin M, Stevenson LW , et al. Clinical presentation, management, and in-hospital outcomes of patients ad-mitted with acute decompensated heart failure with preserved systolic function a report from the Acute Decompensated Heart Failure Na-tional Registry (ADHERE) Database. J Am Coll Cardiol. 2006;47:76–84. [PubMed] [Google Scholar] 7. Lam CS, Carson PE, Anand IS , et al. Sex differences in clinical characteristics and outcomes in elderly patients with heart failure and preserved ejection fraction the Irbesartan in Heart Failure with Preserved Ejection Fraction (I-PRESERVE) trial. Circ Heart Fail. 2012;5:571–8. [PMC free article] [PubMed] [Google Scholar] 8. Hoekstra T, Lesman-Leegte I, van Veldhuisen DJ, Sanderman R, Jaarsma T. Quality of life is impaired similarly in heart failure patients with preserved and reduced ejection fraction. Eur J Heart Fail. 2011;13:1013–8. [PubMed] [Google Scholar] 9. Yang HX, Hou X, Lin P, Rong TH, Yang H, Fu JH. Survival and risk factors of surgically treated mediastinal inva-sion T4 non-small cell lung cancer. Ann Thorac Surg. 2009;88:372–8. [PubMed] [Google Scholar] 10. Meta-analysis Global Group in Chronic Heart F The survival of patients with heart failure with preserved or reduced left ventricular ejection fraction an individual patient data meta-analysis. Eur Heart J. 2012;33:1750–7. [PubMed] [Google Scholar] 11. Borlaug BA, Paulus WJ. Heart failure with preserved ejection fraction pathophysiology, diagnosis, and treatment. Eur Heart J. 2011;32:670–9. [PMC free article] [PubMed] [Google Scholar] 12. Nagueh SF, Appleton CP, Gillebert TC , et al. Recom-mendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr. 2009;22:107–33. [PubMed] [Google Scholar] 13. Jessup M, Brozena S. Heart failure. N Engl J Med. 2003;348:18. [Google Scholar] 14. European Study Group on Diastolic Heart Failure How to diagnose diastolic heart failure. Eur Heart J. 1998;19:990–1003. [PubMed] [Google Scholar] 15. Guidelines for the evaluation and management of heart failure.Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Evaluation and Management of Heart Failure). Circulation. 1995;92:2764–84. [PubMed] [Google Scholar] 16. Maurer MS, Hummel SL. Heart failure with a preserved ejection fraction what is in a name?. J Am Coll Cardiol. 2011;58:275–7. [PubMed] [Google Scholar] 17. Yu CM, Lin H, Yang H, Kong SL, Zhang Q, Lee SW. Progression of systolic abnormalities in patients with "isolated" diastolic heart failure and diastolic dysfunction. Circulation. 2002;105:1195–201. [PubMed] [Google Scholar] 18. Borlaug BA, Lam CS, Roger VL, Rodeheffer RJ, Redfield MM. Contractility and ventricular systolic stiffening in hypertensive heart disease insights into the pathogenesis of heart failure with preserved ejection fraction. J Am Coll Cardiol. 2009;54:410–8. [PMC free article] [PubMed] [Google Scholar] 19. Borlaug BA, Melenovsky V, Russell SD , et al. Im-paired chronotropic and vasodilator reserves limit exercise capacity in patients with heart failure and a preserved ejection fraction. Circula-tion. 2006;114:2138–47. [PubMed] [Google Scholar] 20. Ennezat PV, Lefetz Y, Marechaux S , et al. Left ven-tricular abnormal response during dynamic exercise in patients with heart failure and preserved left ventricular ejection fraction at rest. J Card Fail. 2008;14:475–80. [PubMed] [Google Scholar] 21. Kawaguchi M, Hay I, Fetics B, Kass DA. Combined ventricular systolic and arterial stiffening in patients with heart failure and preserved ejection fraction implications for systolic and diastolic reserve limitations. Circulation. 2003;107:714–20. [PubMed] [Google Scholar] 22. Brubaker PH, Joo KC, Stewart KP, Fray B, Moore B, Kitzman DW. Chronotropic incompetence and its contribution to exercise intolerance in older heart failure patients. J Cardiopulm Re-habil. 2006;26:86–9. [PubMed] [Google Scholar] 23. Lam CSP, Roger VL, Rodeheffer RJ, Borlaug BA, Enders FT, Redfield MM. Pulmonary hypertension in heart fail-ure with preserved ejection fraction. J Am Coll Cardiol. 2009;53:1119–26. [PMC free article] [PubMed] [Google Scholar] 24. Melenovsky V, Borlaug BA, Rosen B , et al. Cardio-vascular features of heart failure with preserved ejection fraction versus nonfailing hypertensive left ventricular hypertrophy in the urban Baltimore community the role of atrial remodeling/dysfunction. J Am Coll Cardiol. 2007;49:198–207. [PubMed] [Google Scholar] 25. Maurer MS, Burkhoff D, Fried LP, Gottdiener J, King DL, Kitzman DW. Ventricular structure and function in hy-pertensive participants with heart failure and a normal ejection frac-tion the Cardiovascular Health Study. J Am Coll Cardiol. 2007;49:972–81. [PubMed] [Google Scholar] 26. Paulus WJ, van Ballegoij JJ. Treatment of heart failure with normal ejection fraction an inconvenient truth. J Am Coll Cardiol. 2010;55:526–37. [PubMed] [Google Scholar] 27. Prasad A, Hastings JL, Shibata S , et al. Characteriza-tion of static and dynamic left ventricular diastolic function in patients with heart failure with a preserved ejection fraction. Circ Heart Fail. 2010;3:617–26. [PMC free article] [PubMed] [Google Scholar] 28. Anjan VY, Loftus TM, Burke MA , et al. Prevalence, clinical phenotype, and outcomes associated with normal B-type natriuretic Peptide levels in heart failure with preserved ejection frac-tion. Am J Cardiol. 2012;110:870–6. [PMC free article] [PubMed] [Google Scholar] 29. Paulus WJ, Tschope C, Sanderson JE , et al. How to diagnose diastolic heart failure a consensus statement on the diagno-sis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur Heart J. 2007;28:2539–50. [PubMed] [Google Scholar] 30. Vasan RS, Levy D. Defining diastolic heart failure a call for standardized diagnostic criteria. Circulation. 2000;101:2118–21. [PubMed] [Google Scholar] 31. Yturralde RF, Gaasch WH. Diagnostic criteria for dias-tolic heart failure. Prog Cardiovasc Dis. 2005;47:314–9. [PubMed] [Google Scholar] 32. Zile MR, Brutsaert DL. New concepts in diastolic dys-function and diastolic heart failure Part I diagnosis, prognosis, and measurements of diastolic function. Circulation. 2002;105:1387–93. [PubMed] [Google Scholar] 33. Meyer T, Shih J, Aurigemma G. Heart failure with preserved ejection fraction (diastolic dysfunction). Ann Intern Med. 2013;158:ITC5–1-15. [PubMed] [Google Scholar] 34. A Lindenfeld J, Albert NM , et al. Heart Failure Society of HFSA 2010 Comprehensive heart failure practice guideline. J Card Fail. 2010;16:e1–194. [PubMed] [Google Scholar] 35. Jessup M, Abraham WT, Casey DE , et al. 2009 fo-cused update ACCF/AHA Guidelines for the Diagnosis and Man-agement of Heart Failure in Adults a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines developed in collaboration with the Interna-tional Society for Heart and Lung Transplantation. Circulation. 2009;119:1977–2016. [PubMed] [Google Scholar] 36. Maisel AS, Krishnaswamy P, Nowak RM , et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med. 2002;347:161–7. [PubMed] [Google Scholar] 37. Maisel AS, McCord J, Nowak RM , et al. Bedside B-Type natriuretic peptide in the emergency diagnosis of heart failure with reduced or preserved ejection fraction.Results from the Breath-ing Not Properly Multinational Study. J Am Coll Cardiol. 2003;41:2010–7. [PubMed] [Google Scholar] 38. Borlaug BA, Nishimura RA, Sorajja P, Lam CS, Redfield MM. Exercise hemodynamics enhance diagnosis of early heart failure with preserved ejection fraction. Circ Heart Fail. 2010;3:588–95. [PMC free article] [PubMed] [Google Scholar] 39. Iwanaga Y, Nishi I, Furuichi S , et al. B-type natriuretic peptide strongly reflects diastolic wall stress in patients with chronic heart failure comparison between systolic and diastolic heart failure. J Am Coll Cardiol. 2006;47:742–8. [PubMed] [Google Scholar] 40. Bursi F, Weston SA, Redfield MM , et al. Systolic and diastolic heart failure in the community. JAMA. 2006;296:2209–16. [PubMed] [Google Scholar] 41. Kitzman DW, Little WC, Brubaker PH , et al. Patho-physiological characterization of isolated diastolic heart failure in comparison to systolic heart failure. JAMA. 2002;288:2144–50. [PubMed] [Google Scholar] 42. Horwich TB, Hamilton MA, Fonarow GC. B-type natriuretic peptide levels in obese patients with advanced heart failure. J Am Coll Cardiol. 2006;47:85–90. [PubMed] [Google Scholar] 43. Mehra MR, Uber PA, Park MH , et al. Obesity and suppressed B-type natriuretic peptide levels in heart failure. J Am Coll Cardiol. 2004;43:1590–5. [PubMed] [Google Scholar] 44. Strange G, Playford D, Stewart S , et al. Pulmonary hypertension prevalence and mortality in the Armadale echocardiog-raphy cohort. Heart. 2012;98:1805–11. [PMC free article] [PubMed] [Google Scholar] 45. McLaughlin VV, Archer SL, Badesch DB , et al. ACCF/AHA 2009, expert consensus document on pulmonary hyper-tension a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents and the American Heart Association developed in collaboration with the American College of Chest Physicians, American Thoracic Society, Inc. and the Pulmonary Hypertension Association. Circulation. 2009;119:2250–94. [PubMed] [Google Scholar] 46. Shah SJ. Pulmonary hypertension. JAMA. 2012;308:1366–74. [PubMed] [Google Scholar] 47. Ohara T, Ohte N, Little WC. Pulmonary hypertension in heart failure with preserved left ventricular ejection fraction diag-nosis and management. Curr Opin Cardiol. 2012;27:281–7. [PubMed] [Google Scholar] 48. Thenappan T, Shah SJ, Gomberg-Maitland M , et al. Clinical characteristics of pulmonary hypertension in patients with heart failure and preserved ejection fraction. Circ Heart Fail. 2011;4:257–65. [PubMed] [Google Scholar] 49. Willens HJ, Chirinos JA, Gomez-Marin O , et al. Non-invasive differentiation of pulmonary arterial and venous hyperten-sion using conventional and Doppler tissue imaging echocardiog-raphy. J Am Soc Echocardiogr. 2008;21:715–9. [PubMed] [Google Scholar] 50. Borlaug BA, Olson TP, Lam CS , et al. Global cardio-vascular reserve dysfunction in heart failure with preserved ejection fraction. J Am Coll Cardiol. 2010;56:845–54. [PMC free article] [PubMed] [Google Scholar] 51. Kitzman DW, Higginbotham MB, Cobb FR, Sheikh KH, Sullivan MJ. Exercise intolerance in patients with heart failure and preserved left ventricular systolic function failure of the Frank-Starling mechanism. J Am Coll Cardiol. 1991;17:1065–72. [PubMed] [Google Scholar] 52. Burgess MI, Jenkins C, Sharman JE, Marwick TH. Diastolic stress echocardiography hemodynamic validation and clini-cal significance of estimation of ventricular filling pressure with exer-cise. J Am Coll Cardiol. 2006;47:1891–900. [PubMed] [Google Scholar] 53. Judge KW, Pawitan Y, Caldwell J, Gersh BJ, Kenne-dy JW. Congestive heart failure symptoms in patients with pre-served left ventricular systolic function analysis of the CASS regis-try. J Am Coll Cardiol. 1991;18:377–82. [PubMed] [Google Scholar] 54. Choudhury L, Gheorghiade M, Bonow RO. Coronary artery disease in patients with heart failure and preserved systolic function. Am J Cardiol. 2002;89:719–22. [PubMed] [Google Scholar] 55. Shah SJ. Evolving approaches to the management of heart failure with preserved ejection fraction in patients with coronary ar-tery disease. Curr Treat Options Cardiovasc Med. 2010;12:58–75. [PubMed] [Google Scholar] 56. Tschope C, Westermann D. Heart failure with normal ejection fraction.Pathophysilogy diagnosis, and treatment. Herz. 2009;34:89–96. [PubMed] [Google Scholar] 57. Ahmed A, Rich MW, Fleg JL , et al. Effects of digoxin on morbidity and mortality in diastolic heart failure the ancillary digi-talis investigation group trial. Circulation. 2006;114:397–403. [PMC free article] [PubMed] [Google Scholar] 58. Flather MD, Shibata MC, Coats AJ , et al. Randomized trial to determine the effect of nebivolol on mortality and cardiovascu-lar hospital admission in elderly patients with heart failure (SEN-IORS). Eur Heart J. 2005;26:215–25. [PubMed] [Google Scholar] 59. van Veldhuisen DJ, Cohen-Solal A, Bohm M , et al. Beta-blockade with nebivolol in elderly heart failure patients with impaired and preserved left ventricular ejection fraction Data from SENIORS (study of effects of nebivolol intervention on outcomes and rehospitalization in seniors with heart failure). J Am Coll Cardi-ol. 2009;53:2150–8. [PubMed] [Google Scholar] 60. Cleland JG, Tendera M, Adamus J , et al. The perin-dopril in elderly people with chronic heart failure (PEP-CHF) study. Eur Heart J. 2006;27:2338–45. [PubMed] [Google Scholar] 61. Yusuf S, Pfeffer MA, Swedberg K , et al. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction the CHARM-Preserved Trial. Lancet. 2003;362:777–81. [PubMed] [Google Scholar] 62. Massie BM, Carson PE, McMurray JJ , et al. Irbesartan in patients with heart failure and preserved ejection fraction. N Engl J Med. 2008;359:2456–67. [PubMed] [Google Scholar] 63. Edelmann F, Wachter R, Schmidt AG , et al. Effect of spironolactone on diastolic function and exercise capacity in patients with heart failure with preserved ejection fraction the Aldo-DHF randomized controlled trial. JAMA. 2013;309:781–91. [PubMed] [Google Scholar] 64. Liu Y, Haddad T, Dwivedi G. Heart failure with pre-served ejection fraction current understanding and emerging con-cepts. Curr Opin Cardiol. 2013;28:187–96. [PubMed] [Google Scholar] 65. Guazzi M, Vicenzi M, Arena R, Guazzi MD. Pulmo-nary hypertension in heart failure with preserved ejection fraction a target of phosphodiesterase-5 inhibition in a 1-year study. Circula-tion. 2011;124:164–74. [PubMed] [Google Scholar] 66. Redfield MM, Chen HH, Borlaug BA , et al. Effect of Phosphodiesterase-5 inhibition on exercise capacity and clinical sta-tus in heart failure with preserved ejection fraction a randomized clinical trial. JAMA. 2013;309(12):1268–77. [PMC free article] [PubMed] [Google Scholar] 67. Solomon SD, Zile M, Pieske B , et al. The angiotensin receptor neprilysin inhibitor LCZ696 in heart failure with preserved ejection fraction a phase 2 double-blind randomised controlled trial. Lancet. 2012;380:1387–95. [PubMed] [Google Scholar] 68. Omori Y, Ohtani T, Sakata Y , et al. L-Carnitine pre-vents the development of ventricular fibrosis and heart failure with preserved ejection fraction in hypertensive heart disease. J Hypertens. 2012;30:1834–44. [PubMed] [Google Scholar] 69. Reil JC, Hohl M, Reil GH , et al. Heart rate reduction by If-inhibition improves vascular stiffness and left ventricular sys-tolic and diastolic function in a mouse model of heart failure with preserved ejection fraction. Eur Heart J. 2013;34(36):2839–49. [PMC free article] [PubMed] [Google Scholar] 70. Ather S, Chan W, Bozkurt B , et al. Impact of noncardi-ac comorbidities on morbidity and mortality in a predominantly male population with heart failure and preserved versus reduced ejection fraction. J Am Coll Cardiol. 2012;59:998–1005. [PMC free article] [PubMed] [Google Scholar] 71. Shah SJ, Gheorghiade M. Heart failure with preserved ejection fraction treat now by treating comorbidities. JAMA. 2008;300:431–3. [PubMed] [Google Scholar] 72. Kapoor Jr, Heidenreich PA. Heart rate predicts mortality in patients with heart failure and preserved systolic function. J Card Fail. 2010;16:806–11. [PubMed] [Google Scholar] 73. Maeder MT, Kaye DM. Differential impact of heart rate and blood pressure on outcome in patients with heart failure with reduced versus preserved left ventricular ejection fraction. Int J Car-diol. 2012;155:249–56. [PubMed] [Google Scholar] 74. Massie BM, Nelson JJ, Lukas MA , et al. Comparison of outcomes and usefulness of carvedilol across a spectrum of left ventricular ejection fractions in patients with heart failure in clinical practice. Am J Cardiol. 2007;99:1263–8. [PubMed] [Google Scholar] 75. Hernandez AF, Hammill BG, O'Connor CM, Schul-man KA, Curtis LH, Fonarow GC. Clinical effectiveness of beta-blockers in heart failure findings from the OPTIMIZE-HF (Orga-nized program to initiate lifesaving treatment in hospitalized patients with heart failure) registry. J Am Coll Cardiol. 2009;53:184–92. [PMC free article] [PubMed] [Google Scholar] 76. Yamamoto K, Origasa H, Hori M, Investigators JD. Effects of carvedilol on heart failure with preserved ejection fraction the Japanese Diastolic Heart Failure Study (J-DHF). Eur J Heart Fail. 2013;15:110–8. [PubMed] [Google Scholar] 77. Oh JK, Hatle L, Tajik AJ, Little WC. Diastolic heart failure can be diagnosed by comprehensive two-dimensional and Doppler echocardiography. J Am Coll Cardiol. 2006;47:500–6. [PubMed] [Google Scholar] 78. Khandaker MH, Espinosa RE, Nishimura RA , et al. Pericardial disease diagnosis and management. Mayo Clin Proc. 2010;85:572–93. [PMC free article] [PubMed] [Google Scholar] 79. Falk RH. Cardiac amyloidosis a treatable disease, often overlooked. Circulation. 2011;124:1079–85. [PubMed] [Google Scholar] Articles from Current Cardiology Reviews are provided here courtesy of Bentham Science Publishers What is the most common cause of heart failure with preserved ejection fraction?The high prevalence of comorbid cardiovascular disease and cardiovascular risk factors in HFpEF is well recognized (Figure 2). The most prevalent cardiovascular disease in HFpEF is hypertension, which is present in the large majority of HFpEF cases across epidemiological and registry studies.
What does heart failure with preserved EF mean?INTRODUCTION Heart failure with preserved ejection fraction (HFpEF) is a clinical syndrome in which patients have signs and symptoms of HF as the result of high left ventricular (LV) filling pressure despite normal or near normal LV ejection fraction (LVEF; ≥50 percent) [1-5].
What type of heart failure is HFpEF?Heart failure with preserved ejection fraction (HFpEF), also called diastolic failure (or diastolic dysfunction): The left ventricle loses its ability to relax normally (because the muscle has become stiff). The heart can't properly fill with blood during the resting period between each beat.
Which of the following is a feature of heart failure with preserved ejection fraction?Heart failure with preserved ejection fraction is characterized by dynamic impairment of active relaxation and contraction of the left ventricle on exercise and associated with myocardial energy deficiency.
Can you live with heart failure with preserved ejection fraction?A 2017 study found that all people hospitalized with heart failure survived for a median of 2.1 years. Roughly 75 percent of people hospitalized with HFpEF in this study passed away within five years. Cardiovascular and HF readmission rates were higher in those with HFrEF than those with HFpEF.
What is the treatment for heart failure with preserved ejection fraction?Management of HFpEF ranges from lifestyle interventions, (diet, exercise training), management of modifiable risk factors and comorbidities (hypertension, coronary artery disease, atrial fibrillation, obesity, diabetes, cigarette smoking), to pharmacologic therapies, and health services.
|

Related Posts
Advertising
LATEST NEWS
Advertising
Populer
Advertising
About

Copyright © 2024 en.ketajaman Inc.